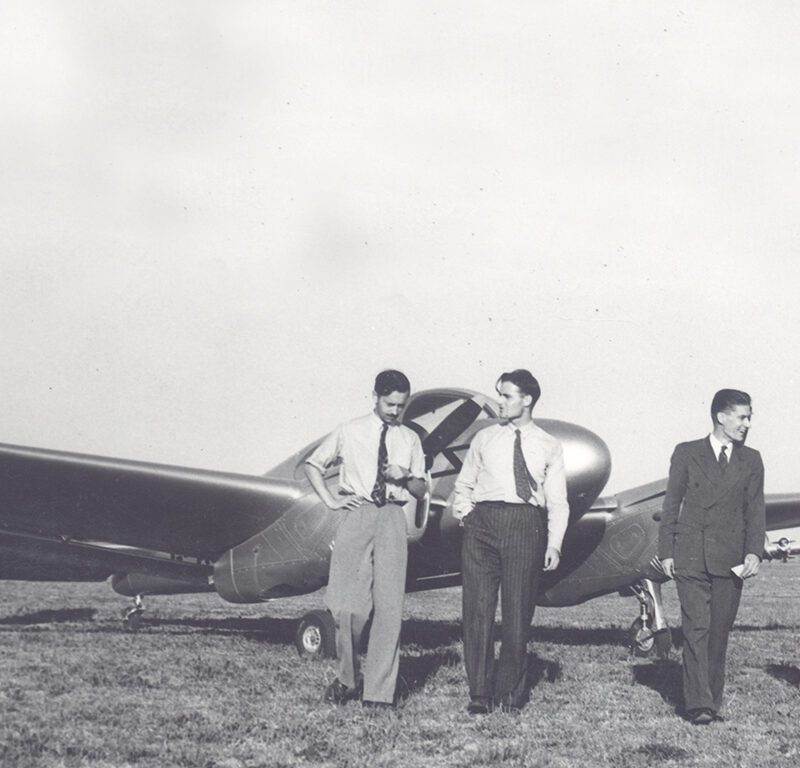
Nepao is pulled from the debris (credit: Mathew Panglas)
It’s a miracle Nepao is alive. Whilst working under his house on 19th August in the remote PNG village of Pyarulama, the stilts holding up his home suddenly gave way on top of him. The weight of the building nearly killed him, but a swift MAF medevac to Kompiam Hospital saved his life. Dr Diana Zwijnenburg has been overseeing Nepao’s recovery…
Houses in rural Papua New Guinea are traditionally built on two-metre stilts to avoid flooding, improve ventilation and to keep out vermin.

A typical house in rural PNG (credit: Dickson Poki)
The area underneath the house also offers much needed respite from the sun – a place in the shade to work on various projects. Unfortunately, Nepao – a married father of two in his late forties – was cutting wood underneath his house when it suddenly collapsed on top of him.
Large fireplace stones from the floor above fell onto his chest and a wooden beam has crushed his leg.
Screaming in pain, he’s pulled from the debris. Mathew Panglas, the local health worker, gives him some morphine and calls for a MAF medevac.
Pilot Mathias Glass medevacks Nepao from Pyarulama to Kompiam Hospital. This mere twelve-minute flight saves his friends from carrying him in a makeshift stretcher over rugged terrain for two days.

Nepao’s house collapses (credit: Matthew Panglas)
Nepao recalls that fateful day:
When the house fell on me, I was covered so people brought axes and knives and cut off the roof. They pulled me out. MAF brought me to hospital and God saved me. My life was given back by God.
Nepao, MAF medevac patient
A&E in the middle of nowhere
Nepao is admitted to Kompiam Hospital just before 5pm. Dr Diana Zwijnenburg, a volunteer doctor from Holland, gets to work on him straight away:
‘He’s badly injured and not very responsive. Although barely conscious, he’s breathing ok. I’m concerned about a possible skull fracture because there’s blood coming from his ear. His right upper leg is broken and there’s a nasty graze and bruising across his chest.’

MAF medevacs Nepao to Kompiam Hospital (credit: Mathias Glass)

Nepao is unloaded from the plane (credit: Mathias Glass)
Unfortunately, the x-ray machine is broken and they’re still waiting for replacement parts:
‘We have an ultrasound machine instead – a real blessing in this situation. Fortunately, there are no collapsed lungs or blood in his abdomen or pelvis, so I’m reasonably confident that there’s no major pelvic fracture.’
In the West, it’s standard practice to protect the neck in all trauma cases, but for doctors like Diana in the middle of the bush with limited resources, there isn’t that luxury:
‘His head has been wobbling around unprotected from the time of the accident. Should I put him in an ill-fitting collar, which might increase the pressure in his head and make a potential skull fracture worse? I decide that is probably worse, so I leave the neck, assuming it’s uninjured.’
Then there’s the other matter of his leg:
‘Under a lot of local anaesthetic, I insert a traction pin into his lower leg and hang some weights on it. This instantly makes his broken leg look a lot straighter.’

Dr Diana Zwijnenburg is Nepao’s doctor (credit: Diana Zwijnenburg)
Nepao takes a turn for the worse
Although Nepao looks better the next day and is fully conscious, bruising on his lungs from the falling stones start to cause breathing problems. Diana is worried:
‘Stones falling from a height of two metres are bound to cause significant damage. I examine him again but can’t find any broken ribs. His condition worsens – by morning he needs nasal prongs to give him oxygen and over the next 24 hours he deteriorates further. By Monday he’s on dual oxygen.’

Nepao is hooked up to a basic ventilator (credit: Diana Zwijnenburg)
Nepao urgently needs a ventilator to survive:
‘We need to intubate him (a breathing tube inserted into the airway) and put him on a ventilator until his lungs have healed enough for him to breathe again on his own.’
This would be an easy decision in the West, but here in the middle of nowhere with few resources, staff have never seen, let alone looked after an intubated patient.
Dr Diana Zwijnenburg, Kompiam Hospital
His family consent to him being put onto a ventilator. Diana has to work fast:
‘I get some stuff together – a simple oxygen powered ventilator, intubation equipment, the suction machine from the labour ward, and various drugs.
‘Two very competent junior doctors and a health care worker are willing to help even though they’re completely outside of their comfort zone. By now, Nepao is on his last few breaths, bathed in sweat from his effort to breathe.’
Divine intervention required!
Diana and the team pray for a miracle:
‘We pray for the God of heaven and earth, the creator and sustainer of life to help. We pray for peace for the family and for a smooth intubation. We pray for this man to live – for God to give him a second chance, so that he can glorify God’s holy name.’
After doing all they can, they leave the rest to God. Nepao stabilises, but needs 24-hour care – an unfamiliar concept to the nurses of rural Papua New Guinea says Diana:
‘I discuss the importance of one nurse being with Nepao at all times. Regardless of lunchtime, breaks or other jobs, he needs to be watched. I realise that most of them don’t know what to watch out for or what to do in case of a problem.
‘Every hour his tube needs to be “suctioned”. More blank faces! Then there’s the matter of regularly turning him, feeding tubes, alarms, the pump and when to get a doctor. The staff have never experienced this before, yet in normal Melanesian fashion, they all nod and say “yes”, indicating their willingness, but I know I will have to show them first.’
With every changeover of staff, Diana patiently explains how to care for Nepao over and over again.

Kompiam is in the middle of mountainous terrain (credit: Diana Zwijnenburg)
Everything is harder in the bush
As if broken equipment and inexperienced medical staff weren’t enough to contend with, there’s also the matter of out-of-date drugs, scarce medical supplies and blocked roads caused by election violence says Diana:
‘In a western Intensive Care Unit (ICU), drugs are administered through different syringes and pumps, which are adjusted to the patient’s needs. Here, we have one pump, so it all goes into one syringe.
‘Next, we realise that we’re going to run out of oxygen bottles before the weekend. Normally we get new supplies, but the road to the provincial capital is blocked due to election violence. Kompiam drivers are not keen to risk it.
‘We’re also running out of bandages, gauzes, and other medications. Two drivers finally pick up some supplies. When they return safely, everyone is so relieved.’
In the meantime, Diana is having issues with the contents of Nepaos syringe and the quality of ICU care:
‘I need to change the contents of his syringe constantly due to some drugs not working properly. Most of our drugs are either 5 to10 years out of date or out of stock altogether.
‘This and the continuous supervision of his care has also become very tiring. One night I found both night nurses fast asleep with nobody watching Nepao. This was quickly rectified and it didn’t happen again.
‘He has also developed some pressure sores because he hasn’t been turned every two hours. We dress all his wounds and turn him to prevent deterioration.’
All this time, Nepao’s family are keeping their distance. Diana learns why:
‘They are terrified. They’re convinced that a bad spirit is to blame – the spirit of Nepao’s wife’s first husband. They blame this spirit for the house collapse and are afraid of more trouble. They also don’t know what’s happened to Nepao’s spirit.
‘The amount of fear is heart-breaking. Our local pastor visits and speaks to them in their own language. Then we pray – God is so much bigger than all these spirits and fears.’

Nepao feeling much better! (credit: Diana Zwijnenburg)
Slow road to recovery
On day five, it appears that Nepao may be able to breathe by himself without a ventilator. Diana is pleased with his progress:
‘His airway pressure has been quite reasonable, and his numbers are looking good. There’s also a lot less debris when suctioning. We get all our equipment ready and stop the sedation. We wait for about three hours but not much happens. Nepao starts to breathe again, but not enough to support himself.
‘The unpredictable effects of the drugs are not helpful. On top of this, the people in PNG seem more sensitive to some of the drugs. I admit defeat and put him back on the ventilator with a different sedative.’
A simple ventilator out in the bush is a lot less sophisticated than ventilators in the West. When it comes to weaning the patient off one, a good ventilator automatically synchronises with the patient’s breathing pattern as the sedative is gradually reduced, but this bush ventilator is unable to do that.
Diana has no choice but to sedate Nepao into a much deeper state of sleep so he can tolerate the ventilator until his lungs are strong enough to breathe on their own.
The disadvantage of this latest sedative is that it runs out much quicker than the previous one explains Diana:
‘Every four hours – day or night – his syringe needs to be changed. After two days, we try again to wean him off the ventilator. We pray again, leaving it all in God’s hands.
‘We stop the syringe and I suction all the debris that he coughs up. Nepao starts to breathe. We stop the ventilator and connect oxygen to the end of his breathing tube.’
Nepao’s breathing is shaky at first, but gradually it improves:
‘Eventually, I take the breathing tube out – he’s on his own. We give him double oxygen and make sure he sits up as much as he can tolerate. We wait – the next hour is crucial.
‘Will he have the energy to sustain his breathing? His lungs are still very stiff and will take effort to overcome the trauma.
‘Two hours later Nepao opens his eyes after a family member calls his name. He improves quickly. Initially confused, Nepao tries to stand on his good leg wondering why his other leg is tied to the bed. He’s reminded that his leg is broken and in traction and is coaxed back to bed.
‘We remove his feeding tube and he’s able to eat and drink. Success! God has done it!’

Nepao with a walking frame – returning home with MAF (credit: Diana Zwijnenburg)
On 25th October, Nepao was discharged from Kompiam Hospital and flown back to Pyarulama by MAF. It was a very emotional experience he says:
‘I cried a lot – I should have died. People shook my hand and cried with me. After sleeping, I killed a pig and gave it to the white people (doctors). I invited them to my house and gave them food. They cared for me and looked after me in hospital. It was a gesture of appreciation. They were there. The plane was there.’
Without the plane, Nepao says he wouldn’t have survived:
I would have died. How could I get to the hospital? It’s not close – it’s far away. Thanks to MAF airlifting me and the work of hospital staff, I am finally leaving this place. May God bless their hands.
Nepao, MAF medevac patient
Without MAF’s medevac, the ending to this story could have been very different.
Join Diana on MAF UK’s ‘Flying for Life’ podcast with Josh Carter. This latest episode explores medevacs and access to healthcare in Timor-Leste, the Democratic Republic of Congo and Papua New Guinea. Diana is joined by MAF pilot Ping Domtta and Maud Kells OBE.
The Flying for Life podcast is a free resource and part of MAF’s ‘He Saw It Was Good’ Bible Study Series, which explores how Christians can support sustainable development.